Introduction:
In recent years, India has faced escalating healthcare expenses, posing a significant challenge for citizens seeking affordable medical care. The Supreme Court of India has recently addressed this issue, emphasising the need for comprehensive healthcare financing reforms beyond just regulating prices. The directive issued by the court in response to a Public Interest Litigation (PIL) highlights the vast disparities in hospital charges, especially evident in procedures like cataract surgeries. This editorial delves into the implications of these developments and explores potential reformative steps that could lead to more equitable healthcare pricing across the nation.
Origin of the Article:
This editorial is based on “Court’s nudge on hospital charges, a reform opportunity” published in The Hindu on April 30, 2024. The article discusses the Supreme Court’s directive to regulate private hospital rates and underscores the urgency of health care financing reforms.
Relevancy for UPSC Students:
Understanding the dynamics of healthcare financing and regulation is crucial for UPSC aspirants. This topic is directly linked to the governance, social justice, and health sectors of the UPSC syllabus, offering insights into the legal frameworks affecting public health policies. Mastery of this subject can aid candidates in writing comprehensive answers in the Mains examination and understanding policy implications in the Prelims.
Overview of the Clinical Establishments (Central Government) Rules, 2012
- Established Authority: Enacted under the Clinical Establishments (Registration and Regulation) Act of 2010, these rules regulate the standardization and operation of clinical establishments across India.
Appointment of the Secretary of the National Council
- Designation and Role: The Secretary, who is an officer of the rank of Joint Secretary dealing with clinical establishments within the Ministry of Health and Family Welfare, acts as the ex-officio Secretary of the National Council.
Role of the National Council
- Classification and Approval: The council classifies and categorizes various clinical establishments and submits their details for approval to the Central Government.
- Formation of Sub-Committees: The council establishes sub-committees with specific roles, ensuring diverse representation from private and public sectors, NGOs, professional bodies, and academia.
Standards for Medical Diagnostic Laboratories
- Compliance with Standards: All clinical establishments must meet minimum standards specified for medical diagnostic services to ensure quality and safety.
Regulations for Displaying Service Rates
- Transparency in Pricing: Clinical establishments are required to clearly display the rates for each service in both local and English languages at visible locations.
Pricing and Compliance
- Regulated Pricing: Establishments must charge within the rate range set by the Central Government, in consultation with State Governments.
- Adherence to Treatment Guidelines: Establishments must comply with Standard Treatment Guidelines issued by the government.
- Maintenance of Records: They are also required to maintain and provide electronic medical or health records as determined by the government.
These structured regulations are designed to improve the accountability, quality, and affordability of healthcare services across the nation, ensuring that all establishments adhere to a common standard of care and transparency.
Overview of Rising Healthcare Costs in India
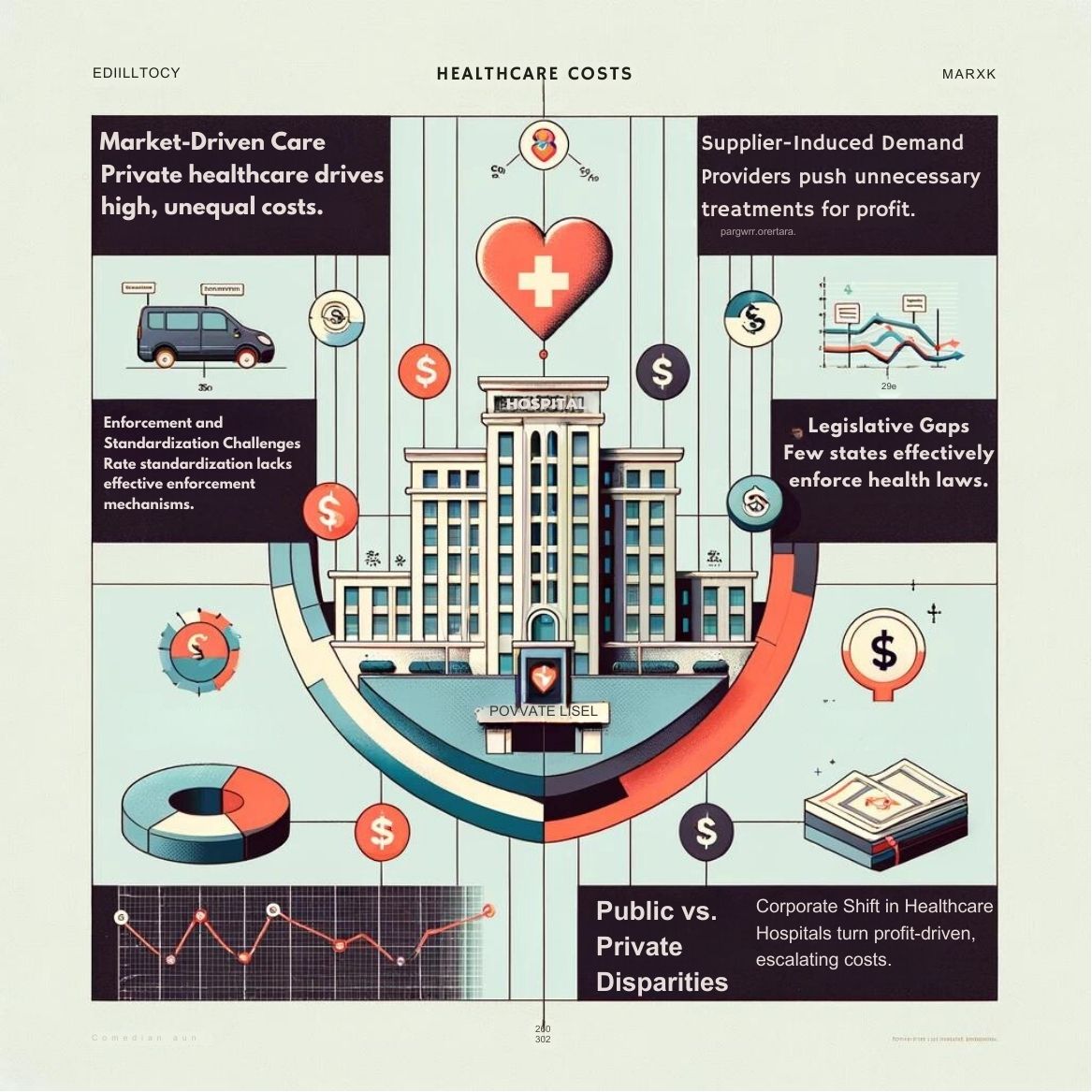
Unregulated and Profit-Oriented Health Sector
- Market-Driven Care: In India, most healthcare is provided by private entities with prices set by the market, leading to high costs and unequal access.
- Supplier-Induced Demand: Healthcare providers may encourage unnecessary treatments to increase profits.
- Challenges of Yardstick Competition: Setting benchmark prices is difficult due to varied patient needs, unreliable data, and weak regulatory frameworks.
High Out-of-Pocket Expenditures (OOPEs)
- Dominance of OOP Payments: Over half of India’s healthcare expenditure comes directly from patients’ pockets, impacting affordability.
- Uncertain Rate Standardization: Even with standard rates, implementation by small-scale private providers remains doubtful.
- Enforcement Issues: Lack of clear mechanisms to ensure providers adhere to set rates, exacerbating cost issues.
Weak Implementation of Laws
- Temporary Impact of Price Caps: Without strong enforcement, price caps only have short-term effects.
- Limited Adoption of Legislation: Only a few states have implemented the Clinical Establishment Act, 2010 effectively, affecting its impact on healthcare affordability and quality.
Issues in Capping Medical Devices
- Ineffective Price Caps: Despite efforts to control prices of essential medical devices, broader systemic issues remain unaddressed.
- Misaligned Stakeholder Incentives: Stakeholders often do not align with the goals of price regulation, undermining its effectiveness.
Corporatisation of Healthcare
- Shift to Profit-Driven Models: Many hospitals have moved from charitable to profit-oriented models, raising costs significantly.
- Few Regulations for Private Practitioners: There is minimal regulation on the fees charged by private doctors, affecting cost transparency and control.
Inadequate Investments in Public Hospitals
- Underfunded Public Sector: Investments in public healthcare are insufficient for the population’s needs, leading to poor service and infrastructure.
- Low Incentives and Infrastructure Issues: Problems like doctor absenteeism and insufficient medical facilities plague public healthcare.
Inadequate Political Priority
- Neglected Healthcare Policy: Despite the potential for low-cost medicines, political inaction and ineffective policies hamper healthcare affordability.
- Urban vs. Rural Disparities: While urban centers may have advanced healthcare, rural areas suffer from underfunded and overcrowded facilities.
These factors collectively contribute to the rising healthcare costs in India, highlighting the need for comprehensive policy reforms and stronger regulatory enforcement to ensure affordable and equitable healthcare access for all citizens.
Various Government Initiatives Related to Healthcare?
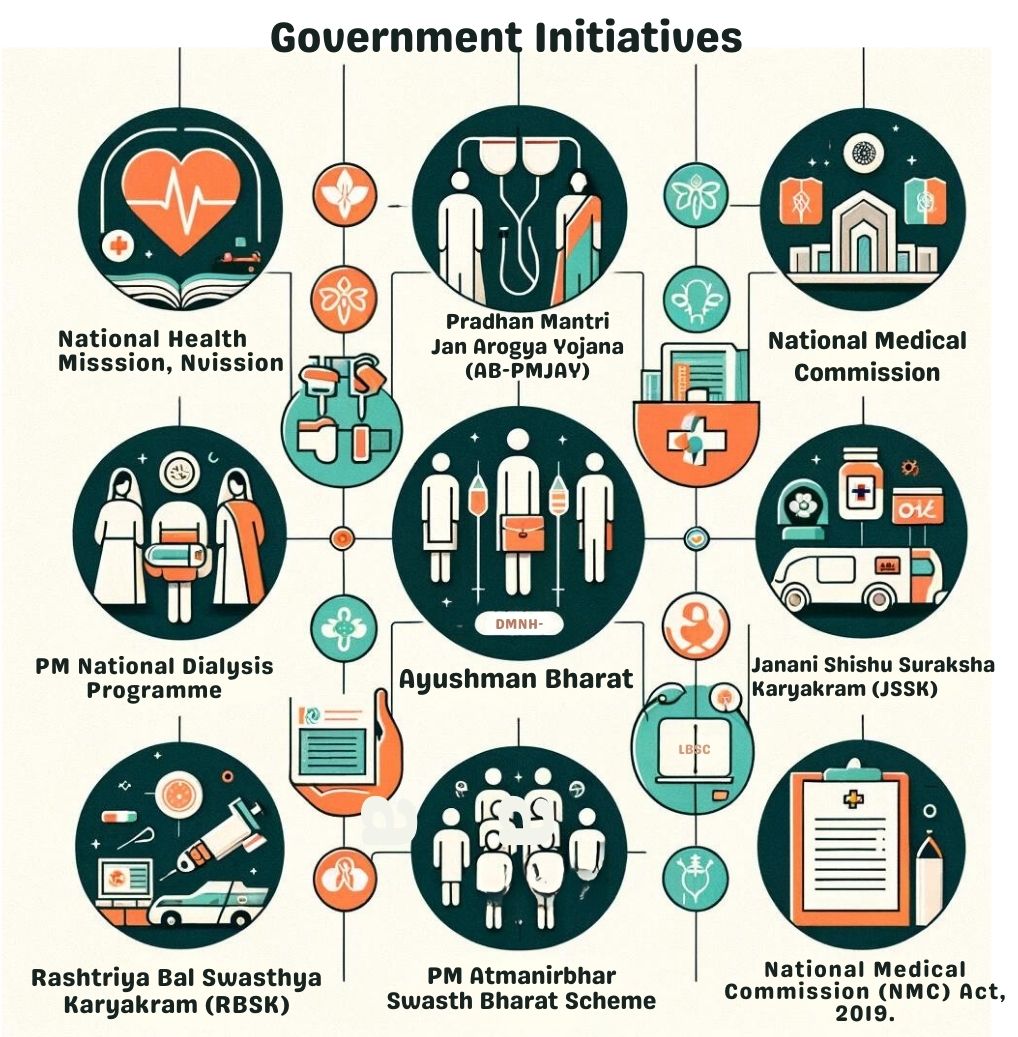
- National Health Mission Ayushman Bharat
- Pradhan Mantri Jan Arogya Yojana (AB-PMJAY)
- National Medical Commission PM
- National Dialysis Programme
- Janani Shishu Suraksha Karyakram (JSSK)
- Rashtriya Bal Swasthya Karyakram (RBSK)
- Increased Allocation for Health in Budget 2021.
- PM Atmanirbhar Swasth Bharat Scheme National
- Digital Health Mission National Medical Commission (NMC) Act, 2019.
- Pradhan Mantri Bhartiya Janaushadhi Pariyojana.
Strategies to Curb Rising Healthcare Costs in India
Formulating Standard Treatment Guidelines (STGs)
- Benchmark for Costs: STGs provide a framework to establish necessary clinical needs and associated costs, ensuring precise valuation of healthcare resources.
- Clinical Autonomy and Care Quality: STGs enable doctors to tailor treatments to individual patient needs while controlling costs.
- Revenue and Payment Reforms: Encouraging providers to accept reimbursements primarily from pooled payments can reduce the burden of out-of-pocket payments.
Comprehensive Health Financing Reform
- Beyond Rate Standardization: A robust health financing strategy is needed to align stakeholder incentives properly and prevent price manipulation.
- Ongoing Research and Standards: Continuous evaluation and updating of benchmark standards are vital to maintain fair pricing and care quality.
Adopting Successful State Models
- Tamil Nadu and Rajasthan’s Approach: These states reduce costs by procuring and distributing unbranded generic medicines directly to patients.
- Expanding Insurance Coverage: Implementing insurance schemes can alleviate out-of-pocket expenses significantly, particularly in a privatized healthcare system.
Transparency in Healthcare Pricing
- Mandatory Rate Display: Regulations require that healthcare providers display their service rates transparently to promote fair pricing.
- Enforcement of Legal Provisions: Despite existing laws like the Clinical Establishments Rules of 2012, there is a significant lag in implementation that needs addressing.
Preventing Irrational Healthcare Interventions
- Standard Protocols: Establishing and enforcing protocols to prevent unnecessary medical procedures, such as excessively high rates of caesarean sections in private hospitals.
- Improving Healthcare Outcomes: Rationalizing treatment practices can significantly reduce costs and enhance patient care quality.
Implementing Patients’ Rights
- Rights to Information and Consent: Patients must have access to information about their condition, treatment options, and costs, and the right to obtain second opinions and choose their providers.
- Grievance Redressal Mechanisms: Establishing effective systems to handle patient complaints, especially regarding private healthcare providers.
Controlling Commercialization in Medical Education
- Fee Regulation in Private Colleges: Mandating that fees in private medical colleges should not exceed those in government institutions.
- Focus on Public Medical Education: Prioritizing the expansion of public medical colleges over commercialized private ones.
Reforming National Medical Commission and NEET
- Independent Review of NMC: The National Medical Commission should undergo a reform to ensure it represents a broad range of stakeholders and decentralizes decision-making.
- Restructuring NEET: Addressing the disadvantages faced by less privileged candidates and respecting state autonomy in medical education processes.
These measures collectively aim to address the multifaceted challenges of rising healthcare costs in India, ensuring a more equitable, efficient, and patient-centered healthcare system.
Way Forward
UPSC aspirants should critically analyze the effectiveness of healthcare regulations and financing reforms in controlling hospital costs. Understanding the dynamics between policy formulation, stakeholder alignment, and enforcement mechanisms is essential for envisaging sustainable solutions to the challenge of rising healthcare prices in India.
Conclusion
In conclusion, tackling the rise in healthcare costs in India requires a holistic strategy that blends regulation, innovation, and transparency. By studying the integration of comprehensive policies and enforcement measures, UPSC aspirants can contribute to shaping a healthcare system that not only controls costs but also improves access and quality for every citizen. This knowledge will be invaluable in their future roles as policy makers and administrators.