The recent World Health Assembly highlighted the complexities of global health governance, focusing on the need for a pandemic treaty. Discussions were intense, especially around equitable access to vaccines, pathogen sharing, and the One Health approach, which links human, animal, and environmental health. Despite progress, the adoption of the treaty remains uncertain due to disagreements on these critical issues. Developing nations, including India, seek fair access to medical resources and technology transfers, emphasizing the need for international solidarity to enhance global pandemic preparedness and health equity.
Origin of the Article
This editorial is based on “The global struggle for a pandemic treaty” published in The Hindu on August 1, 2024. The article discusses the failure of WHO member states to finalize a historic Pandemic Agreement, emphasizing the need for international cooperation.
Relevancy for UPSC Students
For UPSC students, this topic is crucial as it intersects with key areas of the GS Paper 2 and GS Paper 3 syllabi, such as international institutions, government policies, and health governance. Understanding these issues helps in grasping the global health landscape and India’s strategic role, aiding in both Prelims and Mains preparation.

Why in News
The failure of WHO member states to finalize a historic Pandemic Agreement has thrust global health governance into the spotlight. This issue is pertinent for UPSC aspirants, as it intertwines with GS Paper-2 and GS Paper-3 topics such as government policies, international institutions, and health interventions. Understanding the complexities of pathogen access, benefit-sharing, and the One Health approach is crucial, given the previously asked questions on global health equity and pandemic preparedness in the UPSC exam.
Major Health Challenges Currently Affecting the Globe
Introduction: The world today faces a myriad of health challenges that affect populations across different regions. These challenges range from chronic diseases such as cardiovascular conditions to infectious diseases and mental health disorders, presenting a complex landscape for global health governance.
Cardiovascular Diseases
Cardiovascular diseases (CVDs) are a leading cause of mortality worldwide, particularly impacting low- and middle-income countries. In 2021, CVDs accounted for 20.5 million deaths globally, with 80% occurring in these regions. In India, CVDs are responsible for over 26% of all deaths, highlighting the urgent need for effective prevention and management strategies.
Infectious Diseases
Infectious diseases remain a significant challenge despite advancements in medical science. Malaria affects over 200 million people annually, primarily in Africa. HIV/AIDS continues to impact 39.9 million people globally, while tuberculosis caused 1.3 million deaths in 2022. In India, drug-resistant infections lead to over 58,000 newborn deaths each year, with states like Tripura reporting 1,500 new HIV/AIDS cases annually.
Mental Health Disorders
Mental health disorders, including depression and anxiety, affect one in eight people globally, imposing a substantial economic burden estimated to reach USD 6 trillion by 2030. The treatment gap is significant, with 75% of affected individuals in low- and middle-income countries receiving no care. In India, approximately 150 million people require mental health interventions.
Malnutrition and Obesity
The world faces the dual challenge of undernutrition and obesity. In 2022, 2.5 billion adults were overweight, and 890 million were obese, while 390 million were underweight. Childhood malnutrition causes 3.1 million deaths annually, and childhood obesity has surged tenfold over four decades, straining healthcare systems, especially in developing countries.
Non-Communicable Diseases (NCDs)
Non-communicable diseases like cancer, diabetes, and chronic respiratory diseases account for 71% of global deaths annually. The burden is rising rapidly in low- and middle-income countries, where 85% of premature NCD deaths occur. In India, there are 77 million diabetics, with economic losses due to NCDs projected at USD 4.58 trillion between 2012 and 2030.
Climate Change and Health
Climate change poses a significant threat to global health, contributing to heat-related illnesses, respiratory diseases, and vector-borne diseases. The World Health Organization (WHO) estimates that climate change will cause approximately 250,000 additional deaths annually between 2030 and 2050. Air pollution, closely linked to climate change, causes 7 million premature deaths each year, with 1.67 million deaths in India alone in 2019.
Water, Sanitation, and Hygiene (WASH)
Inadequate access to clean water, sanitation, and hygiene facilities poses severe health risks. Globally, 2.2 billion people lack access to safely managed drinking water, and 4.2 billion lack safely managed sanitation services. This contributes to the spread of waterborne diseases, causing 829,000 deaths annually, and exacerbates malnutrition and economic development challenges.
Aging Population and Healthcare
The global aging population presents profound implications for healthcare systems. By 2050, one in six people worldwide will be over 65, increasing the prevalence of age-related conditions like dementia. In India, the elderly population is projected to rise to 319 million by 2050, necessitating substantial healthcare system adaptations.
PESTEL Analysis
| Political: The editorial highlights the ongoing negotiations for a Pandemic Treaty, reflecting political discord at an international level, especially between developing and developed countries. Concerns over sovereignty and the role of the World Health Organization emphasize the political challenges in reaching a consensus on global health policies. Economic: India, as a major player in pharmaceutical manufacturing, has the economic potential to influence global health markets significantly. The economic burden of non-communicable diseases and mental health issues worldwide underscores the need for economic strategies in healthcare that include both preventive measures and effective treatments. Social: The prevalence of traditional medicine in India presents a sociocultural opportunity to integrate these practices with modern healthcare solutions globally. Additionally, the aging population and widespread malnutrition call for culturally adapted health initiatives and education. Technological: India’s capabilities in digital health could lead to technological advances in healthcare. The disagreements over intellectual property rights and technology transfer during health emergencies highlight the need for balanced technological governance that encourages innovation while ensuring fair access. Environmental: Climate change significantly impacts global health, contributing to respiratory and vector-borne diseases. India’s role could extend to addressing these environmental health challenges through sustainable practices and policies. Legal: The legal debates surrounding the Pandemic Treaty, particularly concerning IP rights and equitable access to medical resources, reflect the complexities of establishing a legal framework that accommodates the diverse needs and capacities of countries globally. |
Lack of Global Consensus on the Pandemic Treaty
Introduction: Achieving global consensus on a Pandemic Treaty remains elusive, with significant disagreements on key issues. These disagreements highlight the complexities of global health governance and the challenges of fostering international cooperation.
Equity and Access to Medical Countermeasures
Equitable access to vaccines, treatments, and diagnostics during pandemics is a central issue. Low- and middle-income countries (LMICs) demand guaranteed access to at least 20% of these resources, while high-income countries are hesitant to make binding commitments. The Covid-19 pandemic exposed stark inequities in vaccine distribution, underscoring the need for more equitable mechanisms.
Intellectual Property Rights and Technology Transfer
The governance of intellectual property (IP) rights and technology transfer is another contentious issue. LMICs advocate for provisions facilitating technology transfer and IP waivers during health emergencies. High-income countries and pharmaceutical companies argue that strong IP protections are essential for innovation and investment in research and development, preferring voluntary mechanisms over mandatory ones.
Financing and Resource Allocation
Debates over financing pandemic preparedness are significant. LMICs call for substantial, predictable funding commitments from wealthy nations to build robust health systems. High-income countries acknowledge the need for support but are cautious about open-ended financial commitments. The creation of a Pandemic Fund has received mixed reactions.
Sovereignty and National Autonomy
Concerns about potential infringements on national sovereignty are prevalent. Discussions about the World Health Organization’s (WHO) authority during health emergencies reveal reluctance among some nations to cede decision-making power to an international body, fearing it could override national policies.
One Health Approach and Multisectoral Coordination
The One Health approach, recognizing the interconnection between human, animal, and environmental health, has mixed reactions. High-income countries support it, while some LMICs view it as an additional burden on strained resources. Implementing this approach across sectors and ensuring it does not divert resources from immediate health needs in resource-limited settings is challenging.
Geopolitical Tensions and Trust Deficit
Broader geopolitical tensions and trust deficits underlie technical disagreements on the Pandemic Treaty. Historical inequities in global health governance and the experiences of the Covid-19 pandemic have heightened suspicions and reinforced divisions. Rebuilding trust and fostering genuine collaboration is crucial for progress.
Role of India in Leading Global Healthcare Efforts
India has the potential to play a significant role in global healthcare efforts by leveraging its strengths in pharmaceutical manufacturing, digital health, traditional medicine, affordable healthcare models, global health security, medical education, and research.
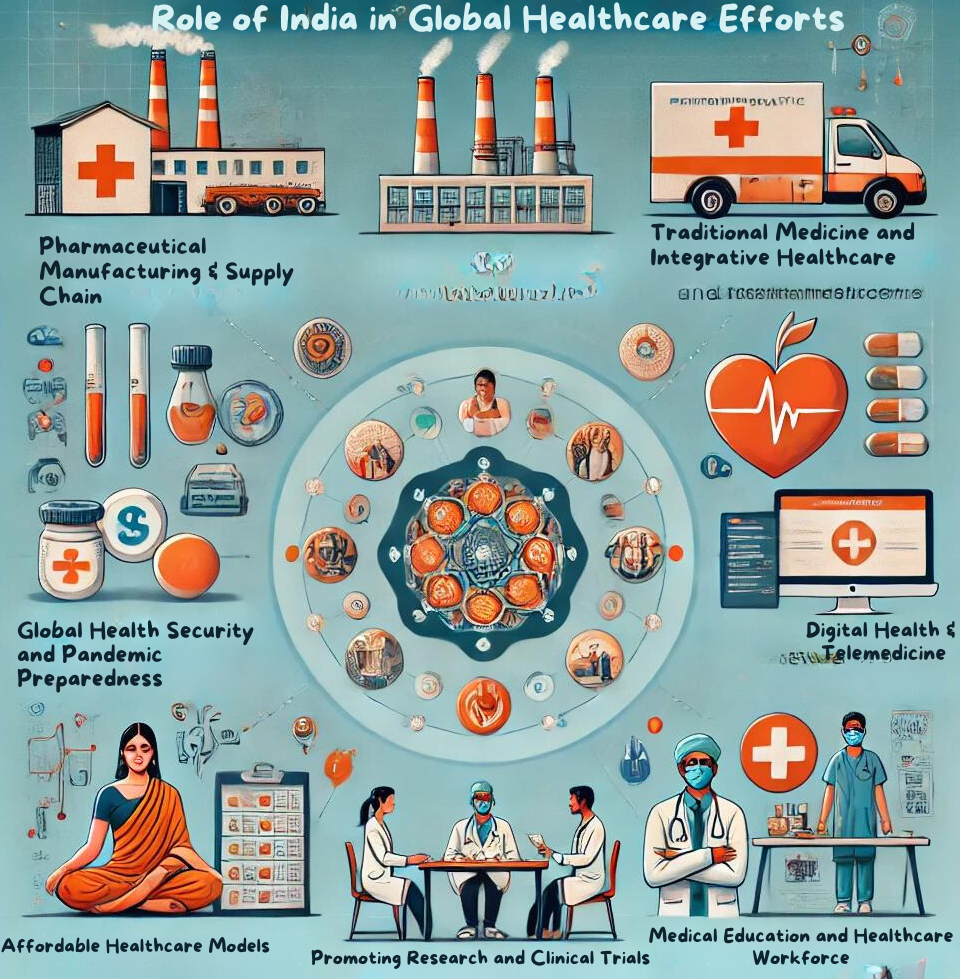
Pharmaceutical Manufacturing and Supply Chain
India should expand and modernize its pharmaceutical manufacturing capabilities to ensure a stable global supply of affordable medicines and vaccines. Investing in research and development is crucial for moving up the value chain. Leveraging schemes like the Production Linked Incentive (PLI) for pharmaceuticals will enhance India’s manufacturing prowess.
Digital Health and Telemedicine
India should capitalize on its digital health initiatives, such as the National Digital Health Mission, to lead in health technology. Sharing expertise in large-scale digital health systems with other developing countries can strengthen this leadership. The success of India’s CoWIN platform for Covid-19 vaccine management is a testament to its potential.
Traditional Medicine and Integrative Healthcare
Promoting evidence-based research in traditional medicine systems like Ayurveda and their integration with modern healthcare can position India as a global authority. Leading efforts in standardizing and regulating traditional medicine practices, supported by the WHO Global Centre for Traditional Medicine in Gujarat, can boost these initiatives.
Affordable Healthcare Models
India should share best practices from large-scale health insurance schemes like Ayushman Bharat with the global community. Promoting innovative, low-cost medical devices and healthcare delivery models can position India as a leader in affordable healthcare, particularly in managing non-communicable diseases in resource-limited settings.
Global Health Security and Pandemic Preparedness
Leveraging its vaccine manufacturing capabilities and infectious disease management experience, India can play a central role in global health security. Contributing to global disease surveillance networks and early warning systems, and sharing expertise in managing diseases like tuberculosis and HIV/AIDS, will be crucial.
Medical Education and Healthcare Workforce
India should lead in developing global standards for medical education and training. Initiating global programs for ethical recruitment and brain circulation, rather than brain drain, will be essential. Building on reforms like the establishment of the National Medical Commission will support these efforts.
Promoting Research and Clinical Trials
Promoting ethical and inclusive clinical trial practices and leading research on diseases prevalent in the Global South can establish India as a key player in global health research. Facilitating global collaborations in medical research, particularly in genomics and personalized medicine, will be crucial.
Conclusion
In conclusion, India’s proactive engagement in global health governance is not just a necessity but a moral imperative. By advocating for equitable access to medical resources, pushing for technology transfers, and implementing the One Health approach, India can lead by example. As future civil servants, your role in shaping these policies will be crucial. Let this inspire you to drive meaningful change on both national and global stages.
| UPSC Civil Services Examination, Previous Year Questions (PYQs) Mains Q. Public health system has limitations in providing universal health coverage. Do you think that the private sector could help in bridging the gap? What other viable alternatives would you suggest? (GS Paper III, 2022). Q. Non-Communicable Diseases (NCDs) are a growing concern globally. Discuss the strategies that India can adopt to address the rising burden of NCDs, with a focus on cardiovascular diseases, diabetes, and cancer. |

